Myelodysplastic Syndrome (MDS)
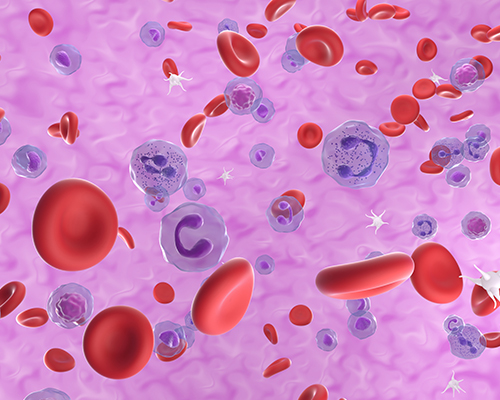
Myelodysplastic syndromes (also called myelodysplasia or MDS) are a rare form of blood cancer, where individuals do not have enough healthy blood cells.
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic neoplasm refers to a group of cancers that hinder blood (hematopoietic) stem cells from maturing into healthy blood cells. Without enough healthy blood cells, individuals may develop serious conditions like anaemia, frequent infections and uncontrolled bleeding. In some case, some individuals with MDS may develop acute myeloid leukaemia (AML).
Types of Myelodysplastic Syndrome
MDS can be classified into various subtypes based on the specific blood cell affected and the severity of the condition. Common subtypes include:
- MDS with Single Lineage Dysplasia
- MDS with Multilineage Dysplasia
- MDS with Excess Blasts
Risks of Myelodysplastic Syndrome
The exact cause of myelodysplastic syndrome (MDS) is often unclear, but certain activities and genetic conditions have been associated with an increased risk of developing MDS.
- Activities Linked to MDS:

Chemical Exposure
Prolonged exposure to certain chemicals, such as benzene, pesticides, and industrial solvents, has been linked to an elevated risk of MDS. Individuals working in industries involving these chemicals may be more susceptible to this condition.

Radiation Exposure
Previous exposure to high levels of ionising radiation, whether due to medical treatments (such as radiation therapy for cancer) or occupational exposure, is a known risk factor for MDS.

Certain Medications
Some chemotherapy drugs used in the treatment of other cancers, particularly alkylating agents and topoisomerase II inhibitors, have been associated with an increased risk of MDS.
- Genetic Conditions Linked to MDS:
Fanconi Anaemia
A rare genetic condition where the bone marrow does not produce enough healthy blood cells.
Diamond-Blackfan Anaemia
A rare genetic condition where the bone marrow does not produce enough red blood cells.
Down Syndrome
Individuals with Down syndrome have an increased risk of developing MDS.
Genetic Mutations
Acquired mutations in specific genes can contribute to the development of MDS. Mutations in genes like TP53, TET2, and ASXL1 have been identified in some cases.
It's important to note that, while these factors are associated with an increased risk, not everyone exposed to these conditions or has these genetic factors will develop MDS. The development of MDS is often a complex interplay of genetic predisposition and environmental factors.
Symptoms of Myelodysplastic Syndrome
The symptoms you have will depend on the type of MDS. For most people, symptoms are mild at first and will slowly get worse.
They can include:
Weakness, tiredness and occasional breathlessness
Frequent infections
Bruising and easy bleeding, such as nosebleeds
Some people with MDS may not experience any symptoms. They may discover they have MDS after undergoing blood tests for other reasons.
Diagnosing Myelodysplastic Syndrome
Diagnosing MPNs involves a combination of medical history reviews, physical examinations, and various tests, including:
Full Blood Count (FBC)
To analyse red and white blood cells, including the number of each white cell type.
Bone Marrow Biopsy
A sample is taken from the bone marrow to look for the abnormalities in the bone marrow cells.
Peripheral Blood Smear
This test will reveal abnormal cell shapes that may indicate a condition. Blood chemistry tests detail the levels of a specific type of chemicals in your blood (proteins, enzymes, glucose, etc.). These numbers provide clues about how your organs are functioning, which may suggest a possible myeloproliferative neoplasm.
Cytogenetic Analysis
To identify changes in your blood cell chromosomes.
